The Gut-Immune System Link
The intricate relationship between our gut and immune system is one of the most exciting frontiers of modern medicine. Our digestive tract isn’t just for breaking down food; it’s the home of trillions of microbes that communicate with and regulate immune cells. In fact, about 70% of the immune system resides here, monitoring invaders and distinguishing them from harmless substances and the body’s own tissues. Celiac treatment strategies, for example, often focus on the gut lining and microbial balance, highlighting the profound interconnection between gut integrity and immune responses in clinical research and patient care. The gut acts as a central command post for immune activity; when it functions optimally, it can suppress unnecessary inflammation and ward off autoimmune attacks. However, its delicate balance can be easily disrupted, making it a crucial player in both protecting against and contributing to disease.
Gut Dysbiosis and Autoimmunity
The balance of beneficial versus harmful bacteria in our gut—a state known as eubiosis—can shift due to factors such as poor diet, antibiotic use, or chronic stress. If this balance is lost, the condition is known as dysbiosis. When dysbiosis develops, harmful bacteria can multiply, crowding out helpful microbes and altering immune signals. Emerging evidence links dysbiosis to the onset or flare-up of various autoimmune diseases, including lupus, multiple sclerosis, and type 1 diabetes. For example, studies have identified specific microbes, such as Enterococcus gallinarum, that can escape from the gut and reach organs like the liver, where they trigger immune reactions that turn the body against itself.
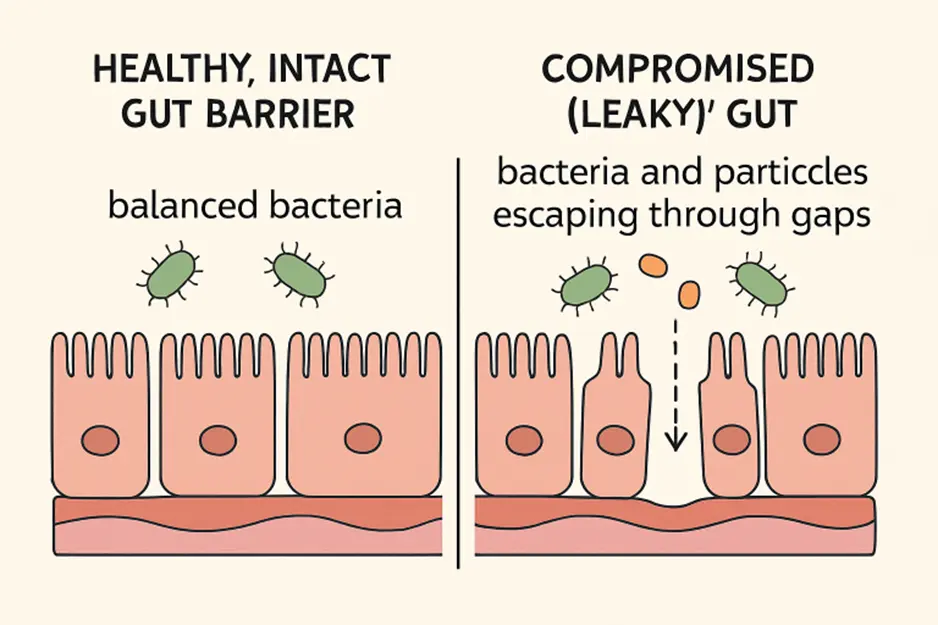
Leaky Gut Syndrome
Leaky gut syndrome—formally known as increased intestinal permeability—occurs when the protective barrier inside the intestines becomes compromised. Typically, tight junctions between intestinal cells prevent bacteria, toxins, and undigested food from entering the bloodstream safely within the gut. When these junctions loosen, foreign particles can leak into the bloodstream. The immune system responds aggressively, thinking it must fight off invaders, but this chronic activation can promote persistent inflammation and ultimately drive autoimmune processes.
Causes of leaky gut can include a high-sugar or high-processed-food diet, chronic stress, certain infections, and even overuse of medications like NSAIDs. This condition doesn’t just affect digestion—it’s an essential factor in seemingly unrelated autoimmune conditions such as rheumatoid arthritis or inflammatory bowel disease.
Diet’s Role in Gut Health
Diet is one of the single most powerful tools for shaping gut health and, by extension, immune function. Diets rich in processed foods and refined sugars create an environment where harmful bacteria thrive, potentially promoting inflammation and disrupting the immune system’s accuracy. In contrast, whole foods—especially those high in fiber, antioxidants, and healthy fats—nourish beneficial bacteria. A plant-forward diet rich in fruits, vegetables, legumes, and whole grains provides prebiotic fibers that nourish protective microbes, thereby enhancing immune tolerance and reducing inflammation. Fermented foods, such as yogurt, kefir, kimchi, and sauerkraut, provide living probiotics that may help restore gut balance. Research has shown that adopting a microbiome-friendly diet can rapidly alter the gut microbiome and may positively influence autoimmune risk.
Probiotics and Prebiotics
Probiotics—beneficial bacteria found in supplements and certain foods—can help replenish and diversify the gut microbiome after it has been disturbed. Prebiotics, such as inulin or fructooligosaccharides found in onions, leeks, and asparagus, are special fibers that act as food for these bacteria. Including prebiotics and probiotics in the diet can strengthen the gut barrier, reduce inflammation, and potentially support better immune tolerance, thereby reducing autoimmune tendencies. Choosing a variety of both, either through supplements or whole foods, may offer specific benefits for immune-mediated conditions. However, individuals with autoimmune diseases or digestive sensitivities should consult with healthcare professionals to tailor their use of probiotics and prebiotics to their unique needs.
Stress and Gut Health
Psychological stress goes far beyond mental discomfort—it can influence what lives in your gut. Chronic stress alters the microbial community and increases the gut’s permeability, boosting the risk for immune system activation. Practicing mind–body activities like meditation, yoga, and deep breathing can modulate stress and enhance both gut and immune system resilience. Ensuring regular physical activity and getting consistent, quality sleep are additional lifestyle levers that help maintain gut health and may be particularly supportive for those facing autoimmune conditions.
Conclusion
Understanding and caring for the gut isn’t just about better digestion—it’s foundational to immune system health and the prevention or management of autoimmune conditions. Small, consistent changes in diet, effective stress management, and thoughtful use of probiotics and prebiotics can all help cultivate a balanced gut ecosystem. Through these approaches, individuals not only support their digestive health but also potentially reduce their risk of autoimmunity and foster overall well-being.
Also Read-Holistic Lab Testing for Better Health Outcomes